Unlock the Power of Personalized Care: Share Your Prescription Us!
- Home
- Knowledgebase
- Medications
- Why is antimicrobial resistance a global concern?
Why is antimicrobial resistance a global concern?
Key facts • Antimicrobial resistance (AMR) is a global health and development threat. It requires urgent multisectoral action in order to achieve the Sustainable Development Goals (SDGs). • WHO has declared that AMR is one of the top 10 global public health threats facing humanity. • Misuse and overuse of antimicrobials are the main drivers in the development of drug-resistant pathogens. • Lack of clean water and sanitation and inadequate infection prevention and control promotes the spread of microbes, some of which can be resistant to antimicrobial treatment. • The cost of AMR to the economy is significant. In addition to death and disability, prolonged illness results in longer hospital stays, the need for more expensive medicines and financial challenges for those impacted. • Without effective antimicrobials, the success of modern medicine in treating infections, including during major surgery and cancer chemotherapy, would be at increased risk.
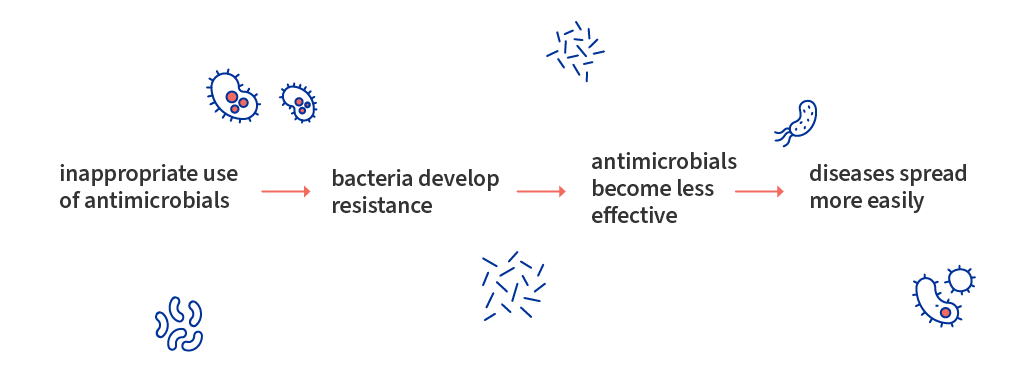
What is antimicrobial resistance? Antimicrobial Resistance (AMR) occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines making infections harder to treat and increasing the risk of disease spread, severe illness and death. As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become increasingly difficult or impossible to treat. Antimicrobial resistance has the potential to affect people at any stage of life, as well as the healthcare, veterinary, and agriculture industries. This makes it one of the world’s most urgent public health problems. Bacteria and fungi do not have to be resistant to every antibiotic or antifungal to be dangerous. Resistance to even one antibiotic can mean serious problems. For example: • Antimicrobial-resistant infections that require the use of second- and third-line treatments can harm patients by causing serious side effects, such as organ failure, and prolong care and recovery, sometimes for months • Many medical advances are dependent on the ability to fight infections using antibiotics, including joint replacements, organ transplants, cancer therapy, and the treatment of chronic diseases like diabetes, asthma, and rheumatoid arthritis • In some cases, these infections have no treatment options If antibiotics and antifungals lose their effectiveness, then we lose the ability to treat infections and control these public health threats. Why is antimicrobial resistance a global concern? The emergence and spread of drug-resistant pathogens that have acquired new resistance mechanisms, leading to antimicrobial resistance, continues to threaten our ability to treat common infections. Especially alarming is the rapid global spread of multi- and pan-resistant bacteria (also known as “superbugs”) that cause infections that are not treatable with existing antimicrobial medicines such as antibiotics. The clinical pipeline of new antimicrobials is dry. In 2019 WHO identified 32 antibiotics in clinical development that address the WHO list of priority pathogens, of which only six were classified as innovative. Furthermore, a lack of access to quality antimicrobials remains a major issue. Antibiotic shortages are affecting countries of all levels of development and especially in health- care systems. Antibiotics are becoming increasingly ineffective as drug-resistance spreads globally leading to more difficult to treat infections and death. New antibacterial are urgently needed – for example, to treat carbapenem-resistant gram-negative bacterial infections as identified in the WHO priority pathogen list. However, if people do not change the way antibiotics are used now, these new antibiotics will suffer the same fate as the current ones and become ineffective. The cost of AMR to national economies and their health systems is significant as it affects productivity of patients or their caretakers through prolonged hospital stays and the need for more expensive and intensive care. Without effective tools for the prevention and adequate treatment of drug-resistant infections and improved access to existing and new quality-assured antimicrobials, the number of people for whom treatment is failing or who die of infections will increase. Medical procedures, such as surgery, including caesarean sections or hip replacements, cancer chemotherapy, and organ transplantation, will become more risk.
What accelerates the emergence and spread of antimicrobial resistance? AMR occurs naturally over time, usually through genetic changes. Antimicrobial resistant organisms are found in people, animals, food, plants and the environment (in water, soil and air). They can spread from person to person or between people and animals, including from food of animal origin. The main drivers of antimicrobial resistance include; a. The misuse and overuse of antimicrobials. Patients should use medicines as prescribed by their physicians. b. Lack of access to clean water, sanitation and hygiene (WASH) for both humans and animals; c. Poor infection and disease prevention and control in health-care facilities. d. Poor access to quality, affordable medicines, vaccines and diagnostics. Most patients due to economy related factors do not get quality medicines and thus e. Lack of awareness and knowledge; and lack of enforcement of legislation. What can we do to stop or reduce the spread of antimicrobial resistance? - Global coordination is needed to both tackle the rise of antimicrobial resistance as well as foster the development of new drugs. We also need to work together to ensure healthcare systems around the world are prepared for rising resistance and infection levels. - Reduce unnecessary use of antimicrobials, it is necessary to use antimicrobials medicines when advised and prescribed by doctors or qualified practitioner. - Improve global surveillance of drug resistance and microbial consumption. Join the NGO’s effort to spearhead the Pharmacovigilance programs. - A global public awareness campaign. It is important that all medicine manufacturers, distributors and dealers collaborate with authorized agencies in respective countries and support the effort to implement public awareness on the proper use of medicines. Credit to: WHO and CDC websites for the information in this posts.
Shop Products
Mebendazole 100
- Study history up to 30 days
- Up to 5 users simultaneously
- Has HEALTH certificate
Flexsa Plus
- Study history up to 30 days
- Up to 5 users simultaneously
- Has HEALTH certificate
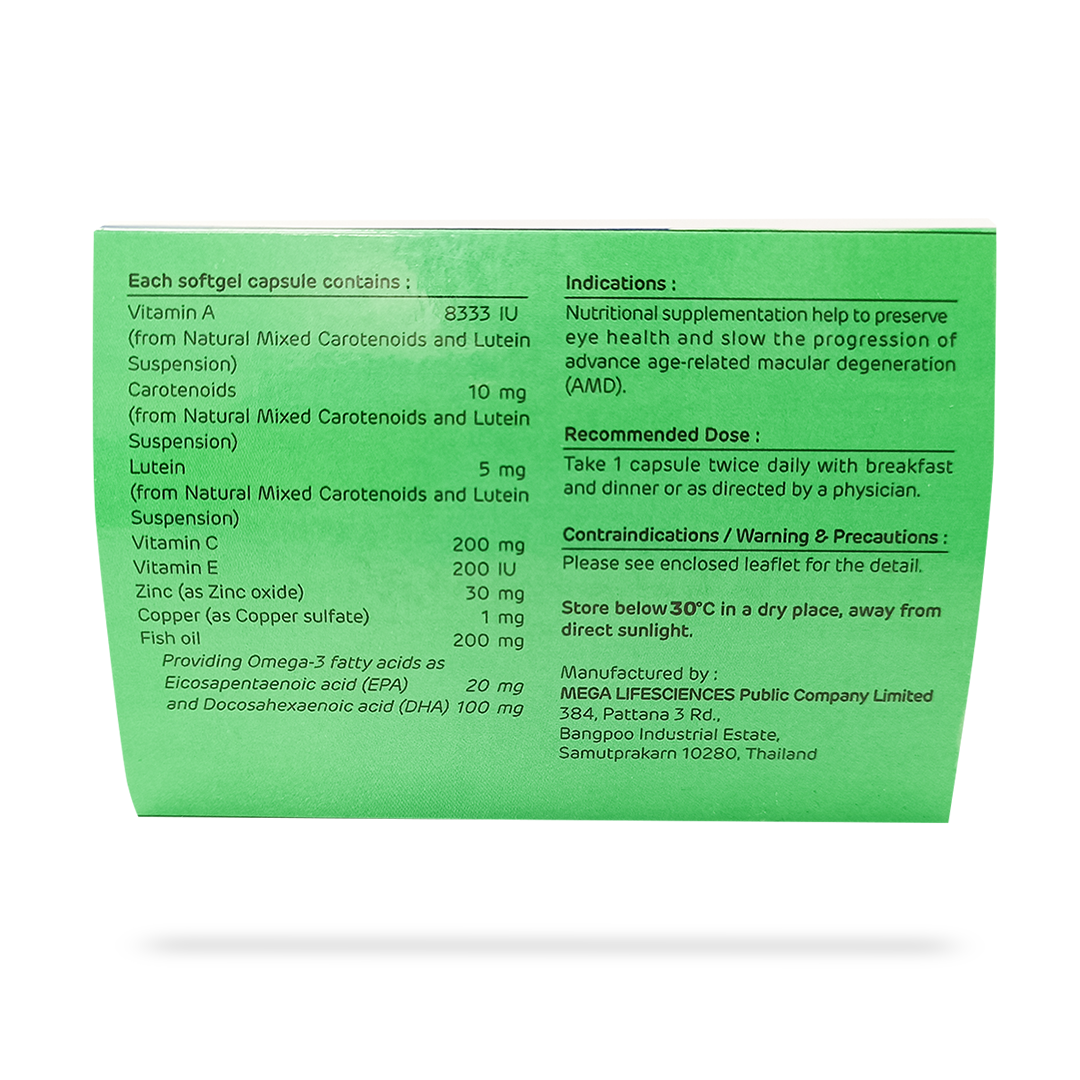
II Care Plus Capsules
- Study history up to 30 days
- Up to 5 users simultaneously
- Has HEALTH certificate
Omega 3 Fish Oil
- Study history up to 30 days
- Up to 5 users simultaneously
- Has HEALTH certificate